The UHC Provider Portal is an online platform that allows healthcare providers to manage administrative tasks with UnitedHealthcare (UHC). It provides real-time access to patient information, claims status, billing data, and more.
Through the portal, providers can securely exchange information with UHC, ensuring faster, more accurate transactions. The UHC Provider Portal is designed to make interactions between healthcare providers and the insurance company more efficient.
Key Features of UHC Provider
The UHC Provider Portal is packed with useful features that can make a significant impact on your practice.
- Eligibility and Benefits Verification: It allows providers to confirm whether a patient’s insurance is active and what services are covered under their plan. Verify the eligibility upfront so providers can avoid claim denials and receive the proper care within their coverage limits.
- Claims Management: Track and manage claims that include submitting claims, checking claim statuses, and viewing payment details. Monitor the claims process in real time, reducing the risk of delays or errors in reimbursement.
- Prior Authorization Requests: UHC requires prior authorization to ensure the service is medically necessary and covered by the patient’s insurance plan.
- Clinical Information Management: The portal provides access to important clinical information, such as lab results and patient notes, helping providers manage their patients’ treatment more effectively.
Set Up the UHC Provider Portal
Here’s a step-by-step guide to help you set up your account and start using its features:
Create an Account
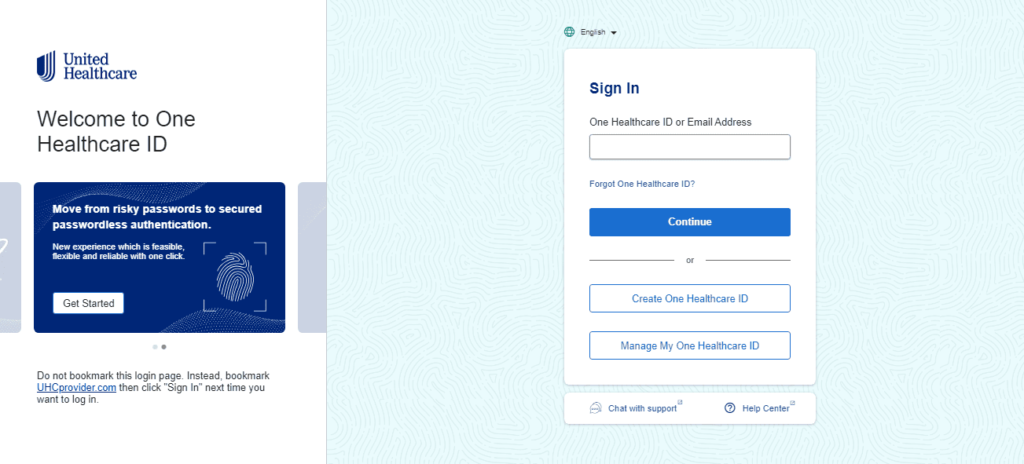
- Visit the UHC Provider Portal.
- Click on the “Sign Up” button.
- Provide your personal details, including the National Provider Identifier (NPI), tax identification number (TIN), and contact information.
Verify your Identity
After entering your information, you will need to verify your identity to protect the confidentiality of patient information. This process typically involves answering security questions or submitting identification documents.
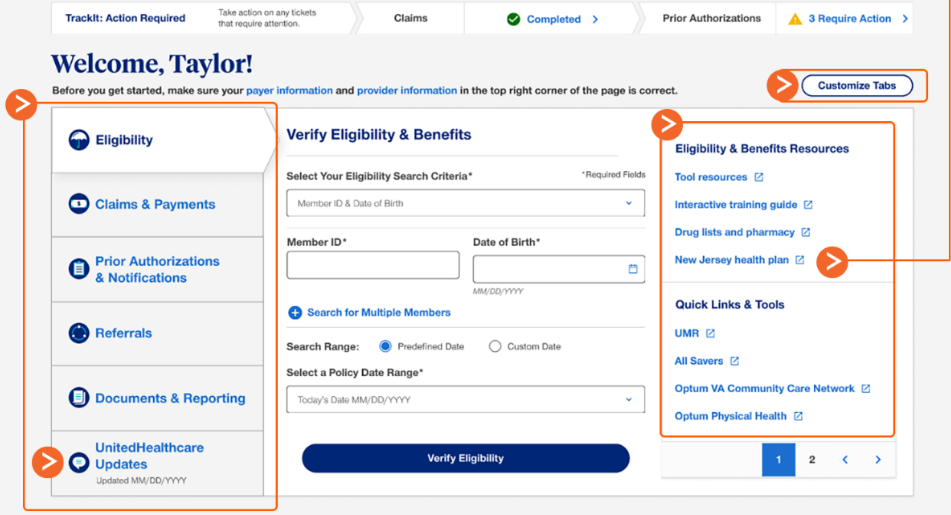
Log In and Familiarize with the Dashboard
Once your account is set up, log into the portal using your username and password. The dashboard is user-friendly and will give you quick access to all the essential tools you need, from claims management to eligibility checks.
Set Up User Roles and Permissions
If your practice has multiple staff members, you can set up different user roles and permissions to control access to sensitive information. This helps ensure that each team member can access the appropriate tools while maintaining patient privacy and security.
Explore Available Resources
Take some time to explore the various resources available in the portal, such as billing guides, FAQs, and provider network directories. These tools will help you optimize your use of the portal and improve your interactions with UHC.
What can you do with UHC Provider Portal?

To make the most of the UHC Provider Portal, here are a few best practices to keep in mind:
- Verify Patient Eligibility Early
Always verify a patient’s eligibility and benefits before providing services. This helps you understand what’s covered and ensures you’re billing correctly, reducing the risk of claim denials. - Track Claims Progress
Regularly monitor the status of your claims in the portal. By doing so, you can address any issues quickly and resolve them before they delay reimbursement. - Submit Prior Authorizations Promptly
Make sure to submit prior authorization requests as early as possible to avoid treatment delays. The sooner you submit these requests, the sooner you’ll receive approval or denial. - Stay Up-to-Date with Coding and Billing Guidelines
Regularly review the latest coding and billing guidelines available in the portal. Staying compliant with UHC’s standards reduces the chance of errors and increases your chances of getting paid on time.
Benefits of Using the UHC Provider Portal
The UHC Provider Portal offers a host of benefits to healthcare providers, including streamlined administrative tasks, improved reimbursement cycles, and better patient care management.
- Time Efficiency and Streamlined Workflow: One of the biggest advantages of the UHC Provider Portal is the time savings it provides. By consolidating multiple administrative tasks into one platform, healthcare providers can reduce the time spent on paperwork.
- Reduced Claim Denials and Errors: Claim denials are one of the most common frustrations for healthcare providers. Errors in coding, eligibility verification, and incorrect information can cause claims to be rejected, resulting in delays or lost revenue.
- Faster Reimbursement and Improved Cash Flow: Delayed reimbursements can create significant cash flow issues for healthcare providers. The UHC Provider Portal helps to speed up the reimbursement process by providing more visibility into the claims and payment process.
- Improved Patient Experience: The UHC Provider Portal not only benefits healthcare providers, but it also improves the overall experience for patients.
The UHC Provider Portal is an essential tool for healthcare providers, offering numerous benefits that improve both the operational side of healthcare delivery and the patient experience.
From faster claims processing and prior authorization approvals to better reimbursement cycles and enhanced data security, the portal allows providers to focus more on patient care.
